Hormonal Health After 40 in Women
Hormonal health after 40 is a transformative and often misunderstood chapter in a woman’s life. Let’s explore what happens, why it matters, and how to thrive, peppered with expert insights, real-life stories, and actionable tips.
Hormonal changes after 40 can leave many women wondering, “What’s happening to my body?” If you’ve noticed mood, sleep, or weight shifts that don’t make sense, you’re not alone.
This article explores the natural hormonal transitions that occur during this stage of life, and most importantly, what you can do to feel your best through it all. You’ll learn how your hormones change in your 40s, what symptoms to watch for, and practical ways to support your body—naturally and medically.
Whether you’re just starting to notice signs or are deep in the throes of perimenopause, this guide offers expert-backed advice and actionable steps. Bonus: Download our free Hormone Health Checklist at the end to help you track your progress and conversations with your doctor.
Understanding Hormonal Shifts After 40
The Broader Hormonal Landscape
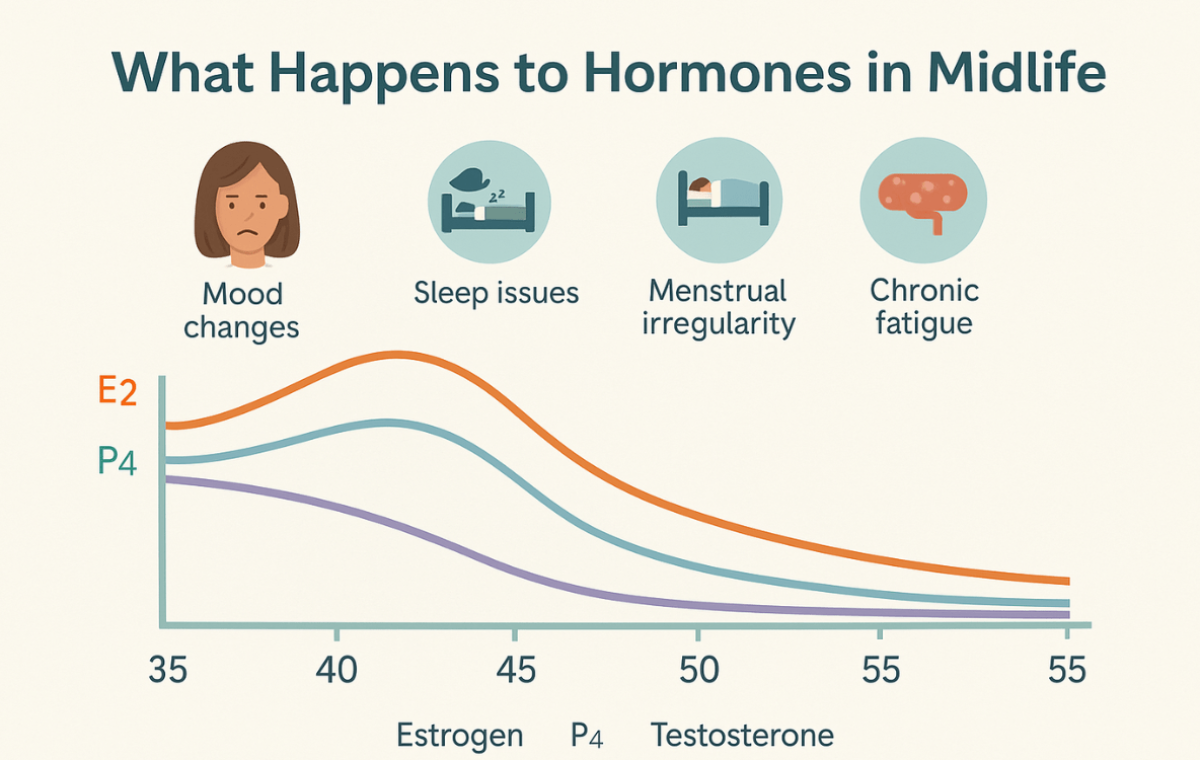
While estrogen and progesterone are central players, hormonal health after 40 also includes other critical hormones like testosterone, thyroid hormones (T3, T4, TSH), and cortisol. These can influence metabolism, energy levels, emotional balance, and body composition. For instance, declining thyroid function—more common in midlife women—can mimic perimenopausal symptoms such as fatigue, weight gain, and depression.
Perimenopause can start as early as the mid-30s and last until the early 50s, depending on genetic and health factors. According to the North American Menopause Society (NAMS), this transition typically spans 4 to 8 years.
[Learn more about perimenopause at the North American Menopause Society.][menopause.org]
Real Stories: Navigating the Transition
Sarah’s Story (Age 47): “I started waking up drenched in sweat and feeling anxious for no reason. At first, I thought it was just stress, but my doctor explained it was perimenopause. Learning this made me feel less alone.”
Lisa’s Journey (Age 44): “My periods became irregular, and I noticed stubborn weight gain. Talking to a nutritionist helped me adjust my diet and feel more in control.”
What Happens to Hormones in Midlife
If you’ve been feeling “off” in your 40s—more tired, moody, or just not yourself—it’s not your imagination. These changes are often tied to natural hormone fluctuations that start to shift as early as your late 30s.
Ovarian vs. Adrenal Hormone Changes
While ovarian hormone changes—like estrogen and progesterone decline—are well known in perimenopause, adrenal hormones also play a role. The adrenal glands help regulate cortisol and produce secondary estrogen after menopause. If these glands are overtaxed due to chronic stress, it can worsen symptoms like fatigue, brain fog, and sleep problems.
Understanding the difference can guide treatment. Ovarian decline usually results in irregular periods and hot flashes, while adrenal fatigue might lead to ongoing low energy, poor stress tolerance, and anxiety, even outside the menstrual cycle. Supporting adrenal health through rest, adaptogens, and stress reduction can complement strategies aimed at ovarian changes.
Estrogen, Progesterone, and Testosterone Decline
Important Health Impact: Menopause can also result in the weakening of the pelvic support structures, increasing the risk of pelvic organ prolapse. Additionally, the loss of bone density during menopause is a major factor in the rise of osteoporosis and fractures among women. (Source: WHO – Menopause Fact Sheet)
Estrogen and progesterone, the two main female hormones, begin to decline during perimenopause. This phase can last for years before the menopause transition officially begins. During this time, hormone levels may swing dramatically from one month to the next, triggering symptoms like irregular periods after 40, breast tenderness, and sudden mood changes. Testosterone also plays a role in libido and energy, and its decline can add to the fatigue and brain fog many women experience.
It’s important to understand that these changes are regular but can affect each woman differently. Some breeze through with minor symptoms, while others may need extra support.
Why Estrogen Matters Everywhere
Estrogen isn’t just about periods—it’s more like your body’s project manager. This hormone keeps tabs on your mood, bones, heart, skin, sleep, and brain function. Scientists now link over 400 body functions to estrogen.² So when levels decline in your 40s, the effects can feel widespread and confusing.
That’s because estrogen decline impacts more than your reproductive system. It plays a starring role in maintaining bone density, regulating cholesterol, and even helping your brain stay sharp.
How Progesterone Affects Sleep & Mood
If estrogen is the multitasker, progesterone is the peacekeeper. This gentle hormone promotes calm, supports deep sleep, and helps counterbalance estrogen’s more energising effects. When progesterone levels start to drop, usually in your early 40s, you might notice changes like anxious thoughts, trouble winding down at night or waking up at 3 a.m.
Progesterone helps produce GABA, a neurotransmitter that relaxes your brain. Without enough of it, your sleep architecture takes a hit. On the mood front, lower progesterone can leave you feeling more emotionally raw or reactive.

Identifying Signs of Hormonal Imbalance
Physical and Emotional Symptoms
Hormonal changes can present with a wide range of symptoms, many of which overlap with other conditions. Here are the most common:
- Hot flashes and night sweats
- Irregular or missed periods
- Mood swings, anxiety, or depression
- Sleep disturbances or insomnia
- Weight gain, especially around the abdomen
- Vaginal dryness and discomfort during sex
- Decreased libido
- Memory lapses or “brain fog”
- Joint pain or stiffness
These symptoms are highly individualised—some women may experience only a few, while others face multiple symptoms with varying intensity. Source: Mayo Clinic, NAMS. Do you ever wonder if what you’re feeling is “just stress” or something more? Hormonal imbalance can mimic many common issues, but there are telltale signs to watch for.
Physically, hot flashes and night sweats, weight gain in midlife women, and changes in hair or skin texture are all red flags. Emotionally, many women experience mood swings and hormones that lead to increased anxiety, irritability, or difficulty concentrating, often referred to as brain fog. These symptoms can creep in gradually, making them easy to dismiss until they start disrupting daily life.
Hormonal Blood Tests for Women
If you suspect a hormone imbalance, don’t guess—get tested. Simple hormonal blood tests for women can reveal your levels of estrogen, progesterone, thyroid hormones, and more. These results can guide the next steps for treatment or lifestyle adjustments.
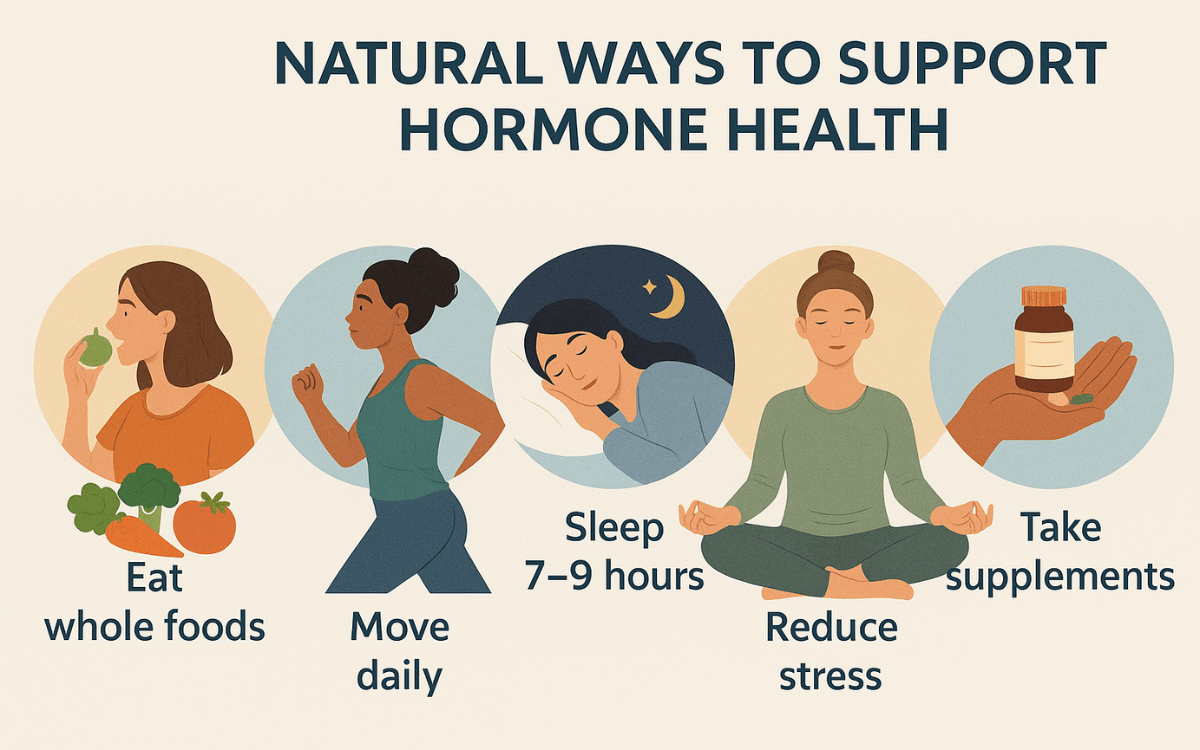
Supporting Hormonal Health Naturally
Expert Tips for Thriving
- Prioritize Nutrition
- Registered dietitian Jessica Cording, MS, RD, advises:
- “Focus on whole foods, lean proteins, and plenty of fibre. Omega-3s from fish or flaxseed can also help with mood and inflammation.”
- Stay Active
- Exercise supports hormone balance, bone health, and mood. Even brisk walking or yoga can make a difference.
- Manage Stress
- Chronic stress raises cortisol, which can worsen hormonal symptoms. Mindfulness, meditation, or simply regular deep breathing can help.
- Sleep Hygiene
- Quality sleep is crucial. Dr. Mary Claire Haver suggests:
- “Create a calming bedtime routine and limit screen time before bed to support your body’s natural rhythms.”
- Seek Support
- Don’t hesitate to talk to your doctor about symptoms. Hormone therapy, non-hormonal medications, and lifestyle changes can all play a role.
Personalised Strategies by Symptom Type
Not all women experience hormonal imbalance the same way, so it’s helpful to tailor support based on your unique symptoms. For example:
- Low libido: Consider boosting testosterone naturally with strength training and maca root.
- Sleep disruption: Magnesium, evening routines, and supporting melatonin production can help.
- Mood swings: Look into adaptogens like ashwagandha, plus consistent blood sugar regulation through diet.
Creating a symptom-based plan empowers women to take specific, targeted steps that match how they feel, not just a one-size-fits-all approach.
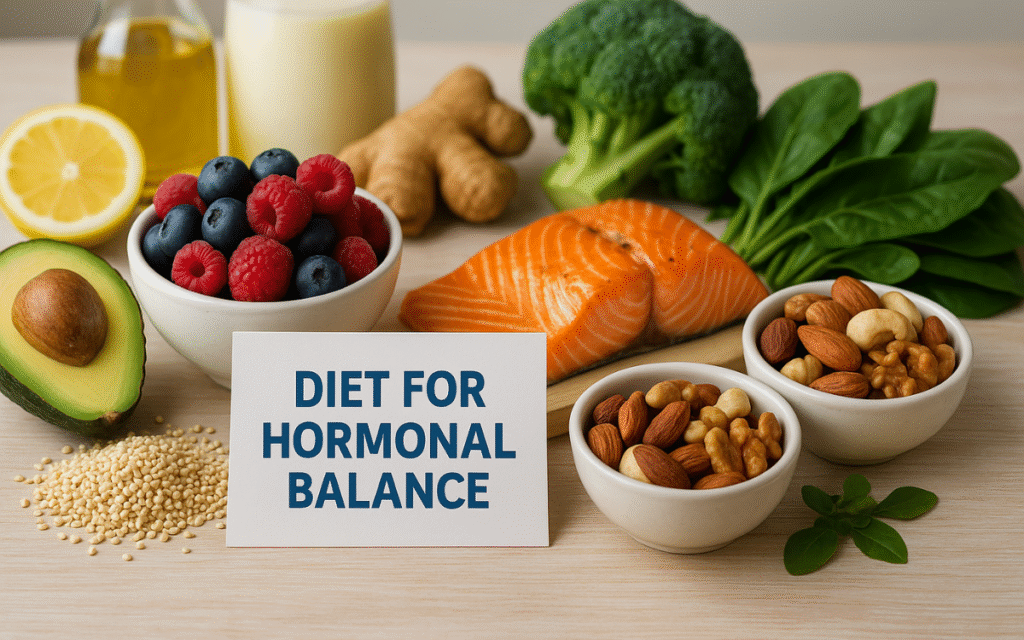
Diet For Hormonal Balance
You don’t have to wait for a diagnosis to take action. Many women find that simple changes in lifestyle and nutrition can make a big difference in how they feel.
Start with food: Eating a diet for hormonal balance, rich in whole foods—especially those containing phytoestrogens (like flaxseeds, soy, and lentils), healthy fats, and omega-3s—can help support estrogen and progesterone balance. Limiting sugar and processed foods also reduces inflammation, which can throw hormones further out of sync.
Exercise, Stress, and Natural Remedies
Exercise and hormone health are closely connected. Strength training helps stabilise insulin and support muscle mass, while walking, yoga, and other low-impact movement can reduce cortisol and improve emotional health during menopause. Add in stress-reducing habits like meditation, journaling, and quality sleep to manage stress in midlife. Some women also benefit from vitamins and supplements for menopause, such as magnesium, maca root, and ashwagandha—though it’s best to consult a provider before starting any new regimen.
Medical and Lifestyle Interventions
Hormone Replacement Therapy (HRT)
Hormone Replacement Therapy (HRT) is one of the most studied treatments for menopause-related symptoms. According to the Endocrine Society and NAMS, HRT is most effective when started within 10 years of menopause onset. It can reduce the risk of osteoporosis, improve quality of life, and alleviate hot flashes and night sweats. However, it’s not suitable for everyone.
Important: Always consult a healthcare provider before starting HRT or any hormonal treatment. Non-hormonal options like selective serotonin reuptake inhibitors (SSRIs), gabapentin, and cognitive behavioural therapy (CBT) are also available and effective for symptoms like mood swings and insomnia. Sometimes, natural strategies aren’t enough—and that’s okay. If symptoms are significantly affecting your quality of life, medical options can offer much-needed relief and restore balance.
Hormone Replacement Therapy (HRT) is a common treatment that replenishes declining hormones, especially estrogen and progesterone. It can be delivered via pills, patches, creams, or other methods. While HRT isn’t for everyone, it can help manage severe symptoms like hot flashes, bone health after menopause, and sleep problems in perimenopause. Always consult a healthcare provider to weigh the benefits and risks based on your personal and family health history.
Holistic Medical Support for Women Over 40
If you’re looking for a more holistic approach, functional or integrative medicine practitioners consider the whole picture—lifestyle, nutrition, genetics, and more. They may use bioidentical hormones or a blend of therapies tailored to your unique needs. Knowing when to see a specialist like an OB/GYN or endocrinologist is a key part of women’s wellness after 40.

My Insight: Embrace the Journey
Having supported many women through the hormonal transitions of their 40s and beyond—as both a health educator and a collaborator with menopause specialists—I’ve witnessed firsthand that this stage can be a powerful time of empowerment and renewal. While the challenges are real, scientific research and clinical experience confirm that with the right knowledge, supportive healthcare, and self-compassion, women can experience a period of renewed vitality and self-discovery.
For example, studies published by the North American Menopause Society show that women who are informed about hormonal changes and actively engage with their healthcare providers report higher satisfaction and quality of life during midlife. In my work, I’ve seen women transform their outlook by embracing evidence-based strategies such as balanced nutrition, regular exercise, and stress management techniques, tailored to their unique needs.
Remember, you’re not alone in this journey. Seeking guidance from trusted professionals, connecting with supportive communities, and staying informed through reputable sources can make all the difference. Menopause is not just an ending, but the beginning of a new, vibrant chapter—one that you have the power to shape.. Yes, there are challenges, but with knowledge, support, and self-compassion, this can be a period of renewed vitality and self-discovery.
Free Tool: Hormone-Aware Weight Loss Quiz
Use this simple tool to learn how your hormone stage might be affecting your weight loss—and get a tailored result immediately.
Final Thought
Hormonal health after 40 isn’t just about managing symptoms—it’s about embracing a new phase with wisdom and strength. Dr. Mary Claire Haver encourages women to see this stage as one of evolution, not loss. In her book The New Menopause, she writes:
“Menopause is not the end of your life; it’s the beginning of a new chapter, and you deserve to feel empowered and informed.”
With this perspective, women can feel more confident and supported in navigating the transition with grace and resilience.
Remember: Every woman’s experience is unique. With the right information and support, you can navigate these changes confidently and thrive in your 40s and beyond.
Hormonal Health FAQs for Women Over 40
Natural support includes food, stress management, and sleep. HRT uses prescription estrogen/progesterone for more direct symptom relief.
They gently mimic estrogen and are linked to fewer hot flashes and better heart and bone markers. Sources: soy, flax, lentils.
Yes, when started early, HRT can protect bones, heart, and possibly reduce risks of Alzheimer’s or colon cancer.
- Eating nutrient-dense, fiber-rich meals
- Strength training regularly
- Practicing stress reduction techniques
- Prioritizing quality sleep
Every woman’s hormonal journey is unique. If you're experiencing unusual or persistent symptoms—like new skin changes, digestive shifts, or sharp mood swings—it’s worth getting your thyroid, cortisol, and sex hormones checked. A personalized approach is always the best route.
TL;DR – What Every Woman Over 40 Needs to Know About Hormonal Health
Hormonal changes in your 40s are real and manageable
Top tools: strength training, gut health, sleep, and possibly HRT
Check thyroid & cortisol if symptoms persist
This isn’t a decline—it’s your power-up phase
Note: Every woman’s experience with menopause and midlife health may differ. Factors like ethnicity, genetics, preexisting conditions, and socioeconomic status can all influence symptoms and outcomes.
✅ Hormonal Health Checklist for Women 40+
| 📌 Action | ✅ Done? |
|---|---|
| Track your symptoms (periods, mood, sleep) | ☑ |
| Get annual thyroid & cortisol screenings | ☑ |
| Eat phytoestrogens (flax, soy, lentils) | ☑ |
| Start strength training 2–3×/week | ☑ |
| Try magnesium or lavender before sleep | ☑ |
| Talk to your doc about HRT options | ☑ |
| Explore CBT or mindfulness for stress | ☑ |
| Prioritize gut health (fiber + fermented foods) | ☑ |
| Follow a Mediterranean-style eating plan | ☑ |